Fibromyalgia Flare Up: Signs, Symptoms, Triggers & Management
August 29, 2025

- A fibromyalgia flare-up may bring widespread pain, fatigue, brain fog, and heightened sensitivity that disrupts daily life.
- Triggers can include stress, poor sleep, weather shifts, or overexertion, though they vary by person.
- Recovery strategies often involve pacing, gentle movement, stress reduction, and prioritizing rest (always guided by a healthcare provider).
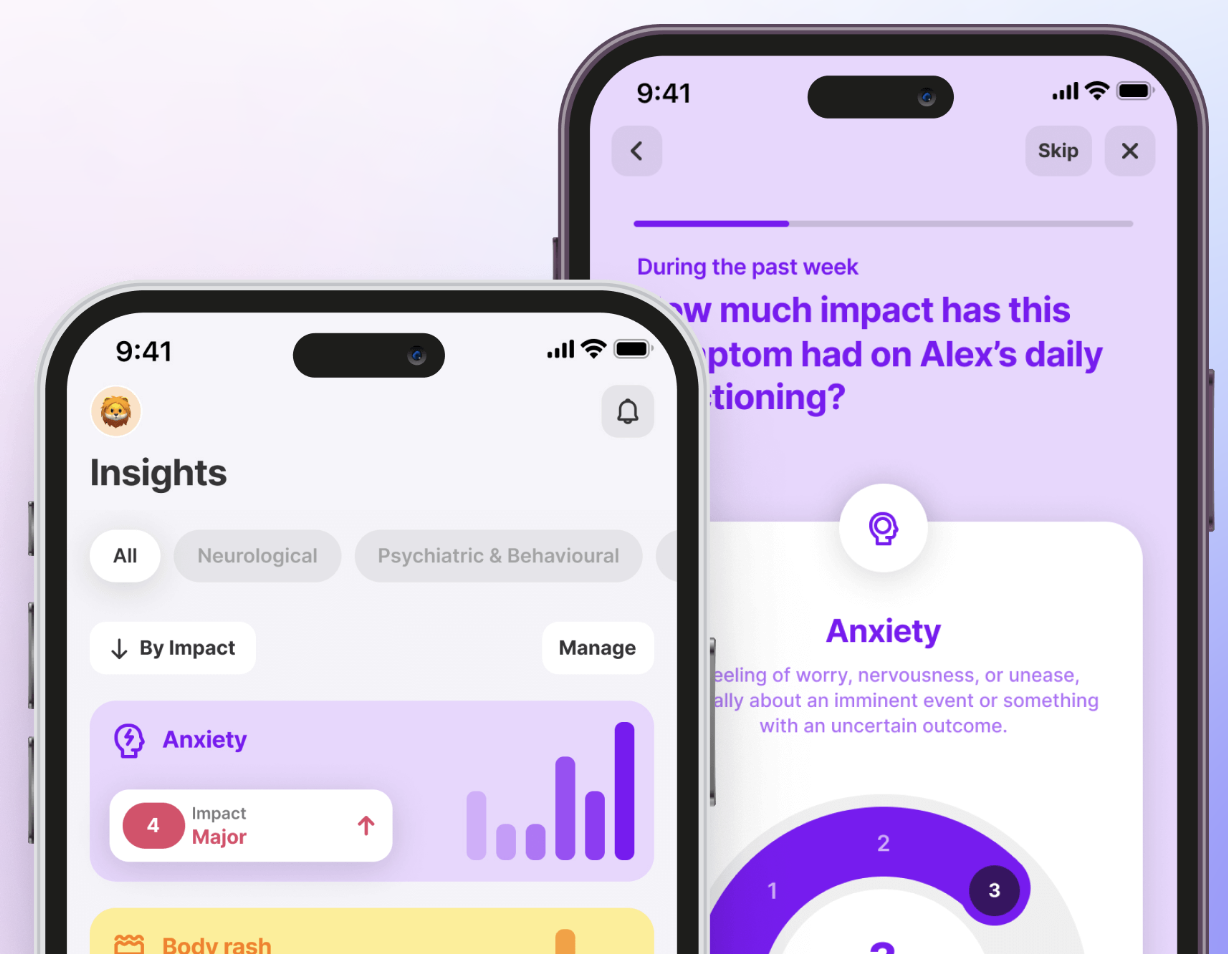
- Tracking symptoms with the Human Health app helps you spot flare patterns, share data with your doctor, and prepare for more informed conversation
Disclaimer: Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information in this article is intended to support, not replace, conversations with qualified healthcare professionals.
Fibromyalgia flare-ups can feel like they strike without warning. One moment you are coping, the next you are weighed down by pain, exhaustion, and brain fog that make daily life harder to manage.
While there is no single way these episodes unfold, knowing the common symptoms and triggers can make them a little less overwhelming.
This article will walk you through what a flare-up looks like, what may cause it, and practical strategies that may help you cope. You will also see how tracking with the Human Health app can help you and your doctor spot meaningful patterns over time.
Symptoms of a fibromyalgia flare-up
Fibromyalgia flares don’t look the same for everyone, but they may involve a combination of physical and cognitive challenges. During a flare, symptoms can intensify, last for days or weeks, and interfere with daily activities.
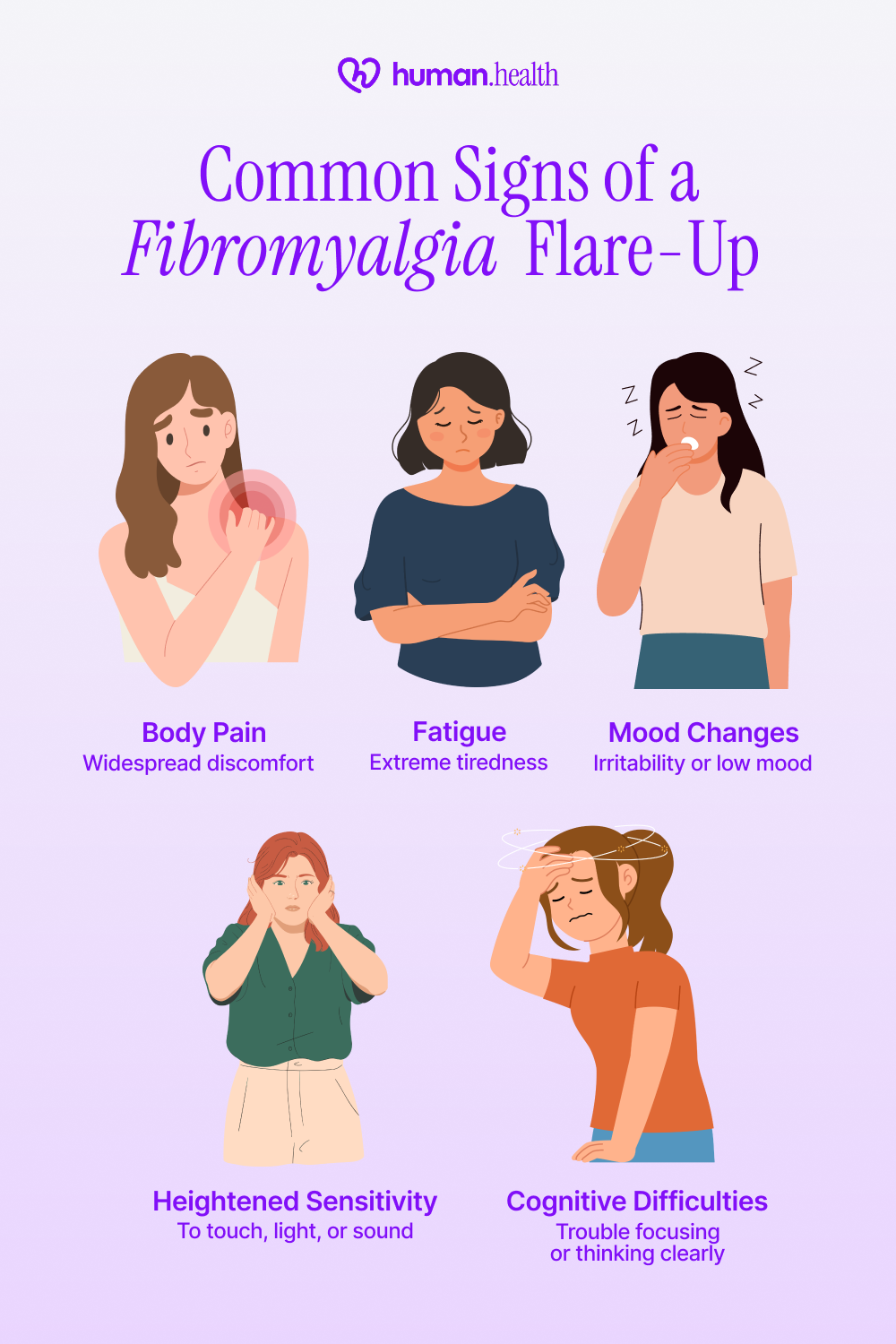
Widespread body pain
A hallmark of flare-ups is deep, aching pain that spreads across muscles and joints. Some people describe it as stabbing, throbbing, or even burning sensations. Pain may shift in intensity and location, often affecting areas such as the shoulders, back, or hips, making it unpredictable and exhausting to manage.
Severe fatigue
Flare-related fatigue is more than being tired; it is a profound lack of energy that persists even after rest or sleep, as reported in studies of women with fibromyalgia.
Even after a full night in bed, sleep may feel unrefreshing. This “non-restorative” sleep can leave you drained, worsening the impact of other symptoms and making daily tasks feel impossible.
Cognitive difficulties (“fibro fog”)
Many people report trouble concentrating, memory lapses, and slowed thinking during flare-ups. This “fibro fog” can include difficulties with multitasking or word-finding, making conversations and work feel frustrating. These lapses are temporary but disruptive, adding mental strain to physical discomfort.
Heightened sensitivity
A flare-up may bring increased sensitivity to touch, sound, light, or temperature changes. Even mild stimuli such as clothing seams, background noise, or strong odors can feel overwhelming. Some people also notice heightened sensitivity to hot or cold environments, which may worsen pain and fatigue.
Mood changes
It is common to experience shifts in mood during flare-ups. These episodes may also affect your mental health, leading to increased anxiety, irritability, or low mood. While not universal, these emotional effects add another layer to flare-up challenges.
By logging these early with the Human Health app's symptom tracker, you may begin to notice patterns in when and how flare-ups start. Bringing those notes to your doctor can help create more informed and productive conversations about your care.
Common triggers of fibromyalgia flare-ups
Flare-ups can sometimes feel unpredictable, but people may notice patterns over time. Recognizing potential triggers is the first step toward reducing their impact.
#1. Stress and emotional strain
Stress is one of the most commonly cited triggers. A large online survey of 2,569 people with fibromyalgia found that 42% reported chronic stress and 31% reported emotional trauma as flare-up triggers. Even seemingly small events, like work frustration or tight schedules, can add up and spark a flare-up. Physical stressors (e.g., illness or injury) may also trigger symptoms.
#2. Poor sleep quality
When sleep is shallow or broken, the body has less chance to repair itself. Many people with fibromyalgia describe waking up just as tired as when they went to bed. Even one or two nights of poor sleep could sometimes tip the balance and trigger a flare-up.
#3. Weather and environmental changes
Shifts in weather, especially changes in barometric pressure, humidity, or cold temperatures, are often reported as flare triggers. Some people notice their symptoms consistently worsen in colder months, while others feel the impact during sudden temperature swings.
{{inline-cta-1}}
#4. Overexertion
Pushing beyond your limits (whether through physical activity, over-scheduling your day, or even mental strain like long hours of concentration) has been identified as a common trigger for flare-ups. Research shows that many people report pain and fatigue intensifying after periods of overexertion.
Tracking these potential triggers with the Human Health app can help you see connections between your daily activities and flare-ups. Over time, these insights may make it easier to prepare for conversations with your healthcare provider and explore supportive adjustments.
How to manage fibromyalgia flare-ups
Managing a flare-up is not about eliminating symptoms overnight. It is about finding ways to ease the intensity in the moment while also building habits that may reduce their impact over time.
What works can be different for everyone, which is why it is important to work with a healthcare provider when exploring options.
#1. Prioritizing rest and pacing
During a flare-up, your body may need more downtime than usual. Breaking activities into smaller chunks, scheduling rest periods, and setting realistic daily goals can help conserve energy and avoid overexertion. Pacing is not about giving up; it is about protecting your reserves so you can get through the flare with less disruption.
#2. Gentle movement and stretching
While it may feel counterintuitive, research shows that light activity, such as stretching, short walks, or gentle yoga, helps ease stiffness and support overall function in people with fibromyalgia.
The key is to move in a way that feels comfortable rather than pushing into pain. Staying entirely inactive for long periods may actually worsen fatigue and make fibromyalgia symptoms feel more severe.
#3. Stress reduction techniques
Stress often amplifies symptoms, so finding calming practices may make a difference. Deep breathing, guided meditation, or simply setting aside quiet time may help calm the nervous system. Even small moments of stress relief can make flare-ups feel less overwhelming.
#4. Heat, cold, or comfort strategies
Simple comfort strategies can provide meaningful short-term relief. Warm baths, heating pads, cooling packs, or creating a quiet, low-stimulation environment are commonly used. These approaches do not remove the flare-up, but they may give you windows of relief that make symptoms easier to handle.
#5. Social and emotional support
Flare-ups can feel isolating, especially when symptoms keep you from your usual activities. Reaching out to supportive friends, family, or communities can provide reassurance and practical help. Emotional support is not a cure, but it can make flare-ups less overwhelming to face.
Lifestyle changes that may reduce flares
Fibromyalgia flare-ups cannot always be prevented, but lifestyle choices can play a role in how frequent or severe they feel. Making small adjustments and staying consistent can give your body more resilience.
#1. Consistent sleep routine
Sleep is often disrupted by fibromyalgia, so building a predictable routine may help improve rest quality. Going to bed and waking up at regular times, keeping the bedroom dark and quiet, and limiting stimulants before bed are all strategies people commonly try. Even modest improvements in sleep may reduce the intensity of next-day symptoms.
#2. Balanced activity levels
Overexertion is a known trigger, but too much rest can worsen stiffness and fatigue. Finding a middle ground is key. Light activities spread throughout the day, alternating effort with breaks, may help maintain stamina without tipping into a flare-up. Planning energy use in advance also gives you more control.
#3. Nutrition and hydration awareness
Some people notice that changes in diet or the use of supplements can influence fibromyalgia symptoms. Research shows that interventions like vitamin D, magnesium, probiotics, and specific dietary approaches may help some patients, although findings are mixed and not universally effective.
Dehydration can also play a role; studies suggest that hydration status influences pain sensitivity in fibromyalgia, with low body water levels linked to increased pain intensity.
While no single diet or hydration strategy is proven to prevent fibromyalgia, staying well-hydrated and paying attention to how meals or treatments relate to your symptoms could offer useful personal insights.
These observations are best discussed with a doctor or nutrition professional, who can help you decide what may be worth adjusting.
#4. Stress management habits
Stress is tightly linked to flare intensity. Building regular stress relief into daily life (whether through meditation, calming hobbies, journaling, or breathing exercises) may help lower your overall stress load. Over time, this can make your body less reactive to common triggers.
#5. Setting boundaries and pacing commitments
Lifestyle changes are not just physical. Saying “no” when your body needs rest, planning lighter days around demanding ones, and pacing social or work commitments could all help reduce flare-up frequency. These boundaries protect energy and prevent the cycle of overexertion followed by collapse.
{{pro-tip-1}}
When to consult with a doctor about your flare-ups
Fibromyalgia flares can sometimes be managed at home, but it’s important to know when to reach out for professional help. If symptoms are escalating, disrupting daily life, or creating new concerns, a healthcare provider should be your next step.
Bringing organized notes to your appointment makes these conversations more productive. The Human Health app lets you track flare frequency, intensity, and triggers over time so you can give your doctor a clearer picture of what you are experiencing.
Stay ahead of flares by tracking triggers and patterns with the Human Health app
Fibromyalgia flares can feel unpredictable, but tracking makes them easier to understand. By logging your symptoms, daily activities, and potential triggers in the Human Health app, you may begin to notice trends that aren’t obvious in the moment.
The Human Health app helps you:
- Log flare intensity, duration, and triggers
- Track treatments for fibromyalgia and lifestyle changes
- Export PDF summaries to share at appointments
Tracking puts you in a stronger position to anticipate flare-ups and have more informed conversations with your healthcare provider.
If you’d like to reflect on how fibromyalgia may be affecting different parts of your daily life, the fibromyalgia FIQR quiz can help you explore your symptom patterns and prepare for a more informed discussion with your healthcare provider.
Ready to take the next step?
Start using the Human Health app today to better understand your patterns and advocate for your care.
FAQs:
#1. Can a fibromyalgia flare mimic other conditions?
Yes, flare symptoms like pain and fatigue can overlap with other illnesses. It’s common for people to wonder about differences between conditions like fibromyalgia vs MS. Only a doctor can confirm whether your symptoms relate to fibromyalgia or something else.
#2. Do fibromyalgia flares follow a predictable pattern?
Some people notice patterns tied to stress, weather, or sleep, but flare timing is highly individual. Tracking consistently may help reveal useful insights to discuss with your provider.
#3. Is it normal to feel emotionally overwhelmed during a flare?
Yes, emotional strain often accompanies physical symptoms. Acknowledging this impact is important, and talking with a healthcare provider may support both emotional and physical well-being.
Sources:
- Oxford Academic, Rheumatology - Treatments for enhancing sleep quality in fibromyalgia: a systematic review and meta-analysis
- National Fibromyalgia Association - Cognitive Function and Fibromyalgia
- The Journal of Rheumatology - Trauma and Fibromyalgia
- National Library of Medicine - Weather conditions and complaints in Fibromyalgia
- National Library of Medicine - Psychological stress and fibromyalgia: a review of the evidence suggesting a neuroendocrine link
- ResearchGate - The Fibromyalgia Syndrome Management- A Short Review on Recent Trends
- National Library of Medicine - Fibromyalgia - StatPearls
- National Library of Medicine - The 4 U’s Rule of Fibromyalgia: A Proposed Model for Fatigue in a Sample of Women with Fibromyalgia: A Qualitative Study
- National Library of Medicine - Psychological impact of fibromyalgia: current perspectives
- National Library of Medicine - Characterizing fibromyalgia flares: a prospective observational study
- National Library of Medicine - Exercise Therapy for Fibromyalgia
- National Library of Medicine - Nutritional Interventions in the Management of Fibromyalgia Syndrome
- National Library of Medicine - Impact of homeostatic body hydration status, evaluated by hemodynamic measures, on different pain sensitization paths to a chronic pain syndrome
Disclaimer
Human Health is a health tracking platform and does not provide medical advice, diagnosis, or treatment. The information on this site is intended to support, not replace, conversations with qualified healthcare professionals.
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.

Track Symptoms & Flare Ups
Better understand your symptoms, and identify triggers that cause symptom changes with the Human Health app.







Pro tip
Choose one lifestyle change to focus on at a time. Tracking too many adjustments at once can be overwhelming, but testing them step by step helps you see what genuinely makes a difference.

.jpg)





.png)

