How does the DSM-5 define OCD?
July 16, 2025

Disclaimer: Human Health is not recommending any specific medical treatment for any particular symptom, nor providing any other medical advice. Always seek the advice of your doctor regarding any medical concern.
Obsessive-compulsive disorder, more commonly known as OCD, is a psychiatric condition experienced by approximately 2.3% of US adults throughout their lifetime. It is characterized by repetitive and persistent thoughts, often accompanied by repetitive behaviors the individual feels compelled to perform in order to relieve the obsessive thoughts.
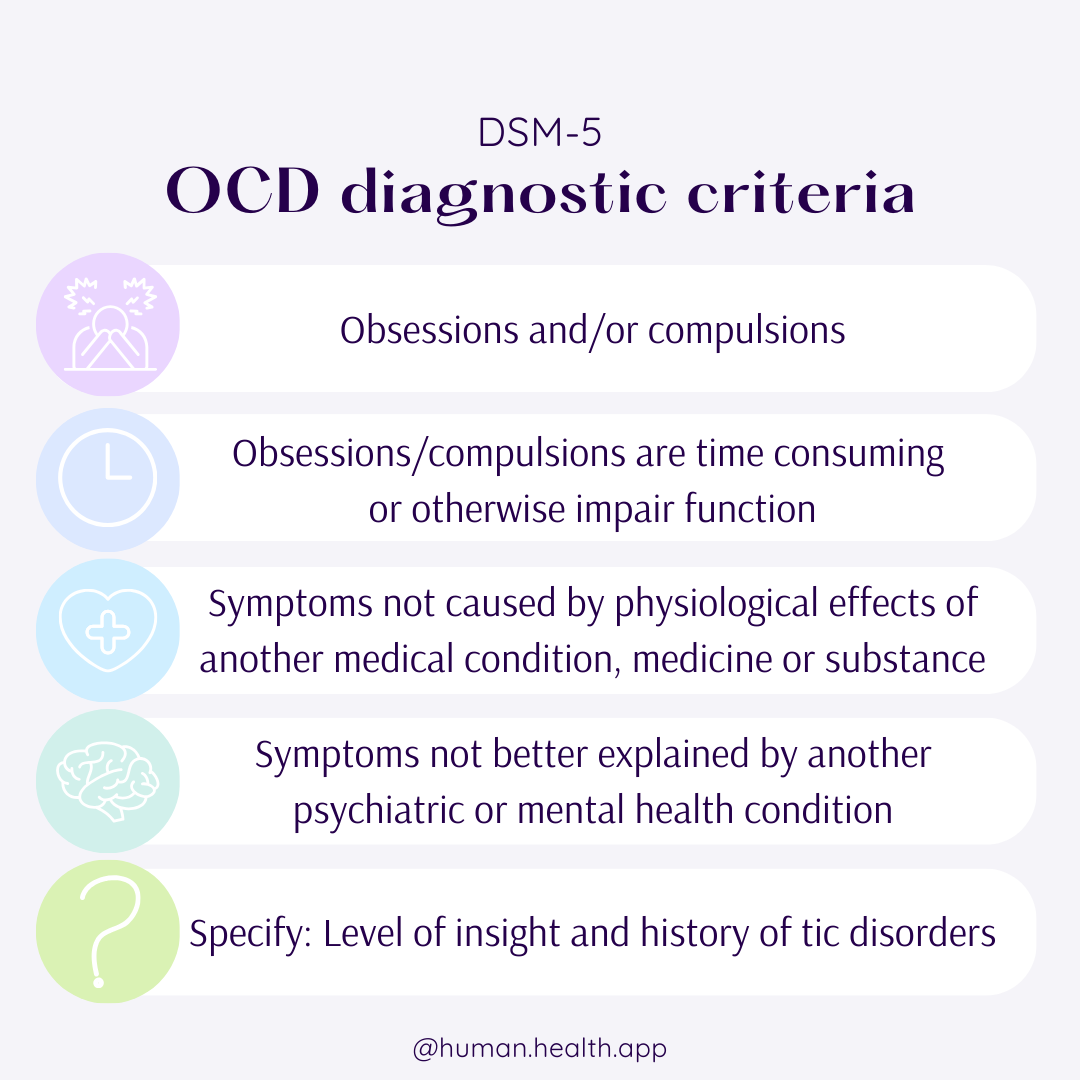
In order to be diagnosed with OCD, patients must meet a specific set of criteria as set by guidelines in the Diagnostic and Statistical Manual (5th Edition), also known as the DSM-5. Usually, patients will be referred to a psychiatrist who will assess their symptoms and whether they meet the threshold for diagnosis.
If you’ve been wondering whether your experiences might align with OCD symptoms, you can take the Obsessive-Compulsive Disorder (OCD) Quiz. This short, evidence-based screener can help you reflect on your thoughts and behaviors before discussing them with a qualified mental health professional.
In this post, we’ll summarise what the DSM-5 criteria for OCD are and what they mean, and we’ve included a visual summary for clarity.
Criterion A
The first criterion specifies that the individual must be experiencing either obsessions, compulsions, or both.
Obsessions are intrusive and unwanted thoughts, urges, or images that occur often and repeatedly, and that do not go away easily. They cause discomfort or distress for the individual, and they may try to ignore them as a result.
Compulsions are the behaviors or mental acts an individual feels they must perform in order to counteract the obsessive thoughts. The individual may feel that performing these rituals will ease their discomfort, make the thoughts go away, or prevent harm or a dreaded event. However, these compulsions may be excessive or unrealistic relative to the actual risk of harm.
Criterion B
To be considered as part of OCD, these obsessions and compulsions must take significant time (e.g., more than 1 hour per day), or considerably impact the individual’s ability to work, socialize, or otherwise function. This is because some level of intrusive thoughts and repetitive behaviors are not uncommon amongst the general population, so it’s important to distinguish if these behaviors fit within the expected range, or are significant enough to be considered as OCD.
Criterion C
The obsessions and compulsions must not be caused by the physiological effects of another medical condition, medical treatment, or substance use. The diagnosing clinician will have to perform a thorough past medical history and examination in order to determine if this is the case, which may take several appointments and information from a variety of sources, such as people close to the patient.
Criterion D
Some other mental health conditions, including anxiety, skin or hair-pulling disorders, eating disorders, and schizophrenia, also present with repetitive or intrusive thoughts and behaviors. To conclude that a patient has OCD, the diagnosing clinician must be sure that their symptoms cannot be better attributed to any other mental health condition. Again, this will involve in-depth history and examination of the patient, and potentially further investigation about any family history of mental health conditions.
Specifiers
Some additional information can be used to further classify the extent and character of a patient’s symptoms. These include the patient’s level of insight and the presence of a tic disorder.
Insight, in medical terms, refers to an individual’s awareness of their illness. For OCD, an individual must be specified to have either:
- Good or fair insight: The patient is aware that their obsessive thoughts are or may be unrealistic or untrue.
- Poor insight: The patient expresses that their obsessive thoughts are probably true.
- Absent insight/delusional beliefs: The patient is insistent and convinced that their obsessive thoughts are true.
To find out how technology can make OCD management easier, read more about our OCD App.
According to the DSM-5, up to 30% of people with OCD also have a tic disorder, which is a condition that results in involuntary movements or sounds. It is important to note if a patient with OCD also has a tic disorder, because it may affect the themes of their obsessive thoughts and compulsions, as well as the pattern of inheritance of the condition, how their condition may develop and change, and their likelihood of developing other conditions.
Thinking about seeking a diagnosis?
Keeping track of your symptoms can be hard, and it can be even harder to remember and recount how they’ve been affecting you when you’re feeling under pressure in your appointments. To make sure you have all the information you need to provide your doctor with an accurate picture of your symptoms, you might like to use a health tracking app.
Human Health is a free mobile app that can help you keep a record of your symptoms and treatments, and provide your doctor with a comprehensive overview of your health journey, from your current concerns to how your symptoms have changed over time.
Click here to download Human Health.
If you liked this article, or think you know someone who might benefit from reading it, please share it! We’d love for our resources to reach those who need them.
Sources
- National Institute of Mental Health. Mental Health Statistics: Obsessive-compulsive disorder (OCD)
- Diagnostic and Statistical Manual of Mental Disorders (5th Edition).
This is a div block with a Webflow interaction that will be triggered when the heading is in the view.










.jpg)





.png)

